Frank Aviles, PT, CWS, FACCWS, CLT
Frank is part of the team evaluating new wound products in the clinic. His previous experience with platelet-rich plasma products and the extensive clinical evidence supporting the effectiveness of 3C Patch® on hard-to-heal diabetic foot ulcers has led to 3C Patch® becoming one of the many wound treatments being offered at Natchitoches Regional Medical Center.
What do you consider to be some of the major challenges in wound care?
I’ve noticed that the wounds are getting more chronic in nature, and this goes hand in hand with the comorbidities present, which complicate the evolution of the wounds.
I started working in wound care in the early ’90s, and it became a passion of mine to get to the root cause of why some patients develop chronic wounds. I noticed that each patient and each wound have a unique constellation of factors, which need to be addressed.
Our team has created a well-defined plan for evaluating these wounds, and the first point of the evaluation is assessing the wound characteristics. When a patient’s wound fails to proceed through the healing cascade, the wound turns chronic.
In the last years, we have seen an explosion of advanced wound care products and technologies on the market, coupled with an overwhelming amount of information regarding wound treatments. This makes it harder for professionals to navigate what products to use on what wounds and when. With a large number of dressings available, I think a major risk is to throw a dressing on a wound, hoping that the wound will improve, without looking at the wound characteristics or trying to address the cause.
Currently, I work with a team of physicians & nurses at an outpatient wound care clinic and other units caring for a large number of patients. My job is to make sure that, as a team, we are attaining set outcomes. It’s my opinion that with more advances in wound care, people tend to forget “the why” and that in approximately 80% of the cases, a wound dressing is meant to complement your treatment intervention and not be the only treatment being offered.
How do you decide what wound care product to use on a specific wound?
When a patient comes to our clinic with a lower extremity wound, we evaluate for adequate perfusion, presence/absence of infection, ongoing trauma, etc. We address these primary issues first to ensure that the procedure or the “ideal” wound dressing selected is an appropriate choice. For example, if there is ongoing trauma to the wound site, it doesn’t matter which dressing we choose – until the trauma is removed, it will likely fail. If there is no perfusion at the wound site, most of the products will fail.
After we do an initial comprehensive evaluation, the data we gather will dictate the treatment protocol. For almost every wound, whether it is venous, diabetic, or pressure injury, data in the literature tells us what the progression of that respective wound should be – in cm2 per week or at the four-week interval.
If, at four weeks, a patient does not meet the benchmarks, our team – that usually includes the nurse manager, the program director, the medical director, and myself- we’ll reevaluate and identify if we are dealing with a hard-to-heal wound. This interdisciplinary team meeting is interesting and educational at the same time since each of us brings a different perspective to the table.
What convinced you to trial 3C Patch® in your clinic?
I was intrigued by 3C Patch® because I’ve already used PRP-like products in the past and had good results with them. Back then, the preparation method meant that we needed to draw blood, mix it, and obtain this gel to apply to a wound.
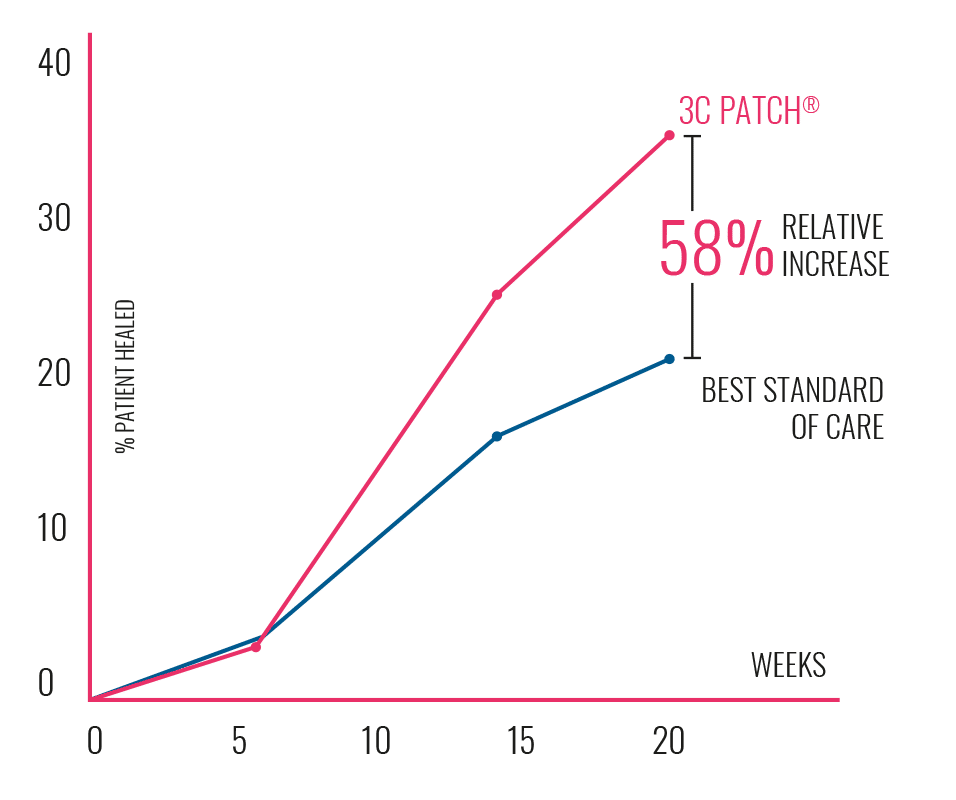
When I learned about 3C Patch®, I knew that the science behind the product is valid and it does work. Furthermore, I was impressed by the technological advancements of the 3C Patch® System. The automated centrifugation process allows for minimal hands-on time, and the resulting patch is easy to apply. This, combined with the fact that 3C Patch® has strong clinical evidence behind it to support its use, were the main factors in trialing the product.


What advanced wound care products and therapies are you using?
We pride ourselves on being an advanced wound care clinic, so we have access to multiple advanced therapies such as negative pressure therapy, low-frequency ultrasound, Hyperbaric Oxygen Therapy, infrared thermography, etc. In terms of cellular-based products, we try to limit the available products in the clinic due to the large number of choices that are available. We usually place them in categories based on their purpose, effectiveness, and available evidence.
3C Patch® is a relatively new advanced wound care product in our clinic, so we are still in the process of defining a category for it. At the moment, we are using 3C Patch® on diabetic foot ulcers that are challenging, difficult to heal, patients that have failed revascularization, or patients that have not responded to other advanced wound care products.
How do you optimize clinic flow when using 3C Patch®?
We are a very busy clinic, so optimizing patient flow is essential for us. The blood is drawn when the patient arrives and placed in the centrifuge. Meanwhile, the physician debrides the wound and, when the patch is ready, it is applied to the wound.
In the beginning, we encountered scheduling issues when several applications occurred simultaneously. This was solved by having two 3CP Centrifuges on site.
The spinning time is not an issue for our clinic because there are always more patients to see, during those 15-20 minutes, while the patch is created in the centrifuge. Furthermore, the doctors and nurses consider that the steps involved in creating a 3C Patch® are reasonably straightforward, and the outcomes we have obtained with this active advanced wound care product are promising. We consider the ease of use and the simplicity of the procedure very advantageous, especially after setting a procedure in place.
What results have you obtained with 3C Patch®?
We have treated ten patients with 3C Patch® so far and are pleased with the results. This advanced product gives us another “tool” for our tool bag as we provide patients with options.
Patient case report
Frank kindly shared, with the patient’s consent, some details regarding the evolution of a wound treated with 3C Patch®. The patient is female with a non-healing diabetic foot wound, originating approximately 14 months prior to arriving at the Natchitoches wound care center. The wound was complicated with pain, severe poor arterial perfusion, and infection. A revascularization referral was made soon after the first visit.

Day 0 - Wound before the first 3C Patch® application
Volume 5.6 cm³

Day 40, after three 3C Patch® applications
Volume 0.13 cm³

Day 83, after a total of six 3C Patch® applications
Volume 0