Martin Johnson
MD
CAN YOU TELL US ABOUT YOUR EXPERIENCE WORKING IN THE WOUND CARE CLINIC?
Our wound clinic is in a tertiary care facility, consequently, our patient population is complicated patients including patients with cancer, organ transplants, and with a diagnosis of 25 plus co-morbidities.
The majority of patients in our outpatient facility suffer from hard-to-heal wounds that have been present for many weeks and most of them have multiple comorbidities. It’s regrettable, especially for patients suffering from diabetes, because they have a higher risk for complications and amputation, which is associated with a decreased 5-year survival.
Studies have compared the life expectancy of 5-year survival in patients with amputation with that of cancer survivors. Only lung cancer and pancreatic cancer have worse 5-year survival than those with amputation due to a diabetic foot ulcer (DFU).
WHAT TYPES OF TREATMENTS/ADVANCED THERAPIES DO YOU PROVIDE FOR PATIENTS WITH HARD-TO-HEAL WOUNDS AND WHAT ARE THE MAIN CRITERIA FOR SELECTING THEM?
We have added advanced dressings (self-adaptive), hypochlorous cleansers/gel, collagen products, we have trialed several CTP (cellular and tissue-based products), and we have implemented the use of the 3C Patch® Technology.
When selecting a new treatment to be added to our practice portfolio we assess a variety of factors including:
- the science behind the product
- the validity of the clinical data
- safety and implementation
- cost-effectiveness
The science must support that a product is an improvement over a product currently on the formulary or offer a new line of therapy. In addition, finances have to support that a product is cost-effective, and it must be safe and able to be used efficiently in an outpatient setting.
Selecting the 3C Patch® was supported by a multicenter, large Randomized Control Study and that was important to present to our product committee. The science (RCT) supports the use of this autologous, automated system to heal our hard to heal DFUs. In addition, regenerative medicine is a pillar of our clinic.
CAN YOU COMMENT ON THE USE OF 3C PATCH® IN CLINICAL PRACTICE?
The 3C Patch® has been well received by both the patients and the staff. When patients are seeing improvement and healing in ulcers that have been present for years or report a 50% reduction in their pain after the first application, there are smiles.
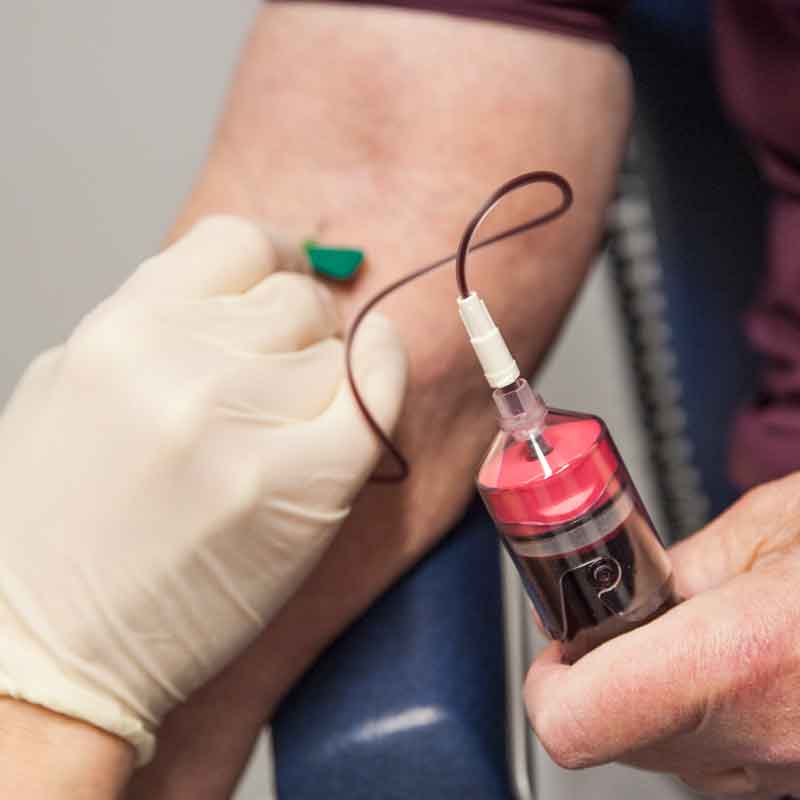
The 3C Patch® System is relatively easy to use, but there are some requirements that need to be in place for the process to run smoothly. You need a nurse who is comfortable drawing blood to be successful, and additional time should be scheduled for difficult blood draws.
CAN YOU DESCRIBE A TREATMENT SESSION WITH 3C PATCH®? WHAT TYPE OF WOUND BED PREPARATION IS NEEDED FOR OPTIMAL EFFECT?
During the first visit of the patient, we assess if the standard of care has been applied and if the wound failed to heal or to progress adequately – I would estimate that around 50% of the patients we see have had a diabetic foot ulcer that had been present for many weeks. In addition, we assess if the 3C Patch® is suitable for this specific patient and wound, and we discuss the treatment protocol with the patient. We also provide additional information that the patient can review after he/she leaves the clinic.
At the next visit, if the patient decided to proceed, we draw 18 ml. of the patient’s blood and place it in the 3CP® Centrifuge. While the blood is spun in the centrifuge to make the 3C Patch®, we prepare the wound bed and the dressing.

On subsequent visits, care is taken to preserve the new epithelium, and additional wound bed debridement might be limited to wound edges or reoccurring callous formation.
In addition to wound bed preparation, another key factor is keeping the 3C Patch® in place until the next visit to ensure that the living cells from the patch stimulate wound healing. Therefore, we secure with sutures often on the plantar location where patient weight-bearing could move the patch. We also use steri-strips to secure the contact layer.
We recommend offloading devices for plantar wounds, ask the patient to stay off the wound as much as possible for 7 days, and ideally, if the patient fits the criteria, we use total contact casting. We have found that the self-adaptive dressing/super-absorptive assists in moisture control and provides additional padding.
WHAT STANDARD OF CARE GUIDELINES SHOULD BE FOLLOWED TO ENSURE OPTIMAL EFFECT OF THE 3C PATCH®?
- Offloading with total contact casting (TCC) is the gold standard and is recommended as long as the patient will tolerate it. A removable system can be used in those patients who don’t tolerate TCC, a knee scooter is another option, or felt podiatry padding can also be used.
- Debridement and wound bed preparation are very important on plantar wounds with a callous build up; this must be addressed to encourage epithelialization across the wound bed.
- Remove epibole at the wound edges. Epibole refers to rolled or curled-under closed wound edges that may be dry, callused, or hyperkeratotic. Epibole tends to be lighter in color than surrounding tissue, has a raised and rounded appearance, and may feel hard, rigid, and indurated.
- Selecting a super absorbent dressing is important. At the initial follow-up visit you must assess the dressing placement, absorption quality of the dressing, and the condition of the periwound to avoid wound maceration. You may need to alter the secondary dressing based on the wound presentation.
- Continuing assessment of the periwound conditions and amounts of wound drainage.
- It is important to secure the primary dressing separate from the secondary dressing to allow for removal and replacement of the secondary dressing, which may be necessary for wounds with moderate to heavy drainage.
WHAT TYPES OF WOUNDS QUALIFY IN YOUR OPINION FOR TREATMENT WITH 3C PATCH®?
As a plastic surgeon, I see applications for venous leg ulcers, arterial ulcers, post-surgical wounds, possible applications in exposed hardware, Mohs defects, radiation wounds. Because you are delivering the patient’s own growth factors and leucocytes, you may consider its use in most hard-to-heal wounds and wounds with decreased blood flow.
